Droopy Tip
Controlling Tip Rotation and Projection
This page summarizes surgical concepts for trainees and colleagues; it is not intended as medical advice.
In addressing the aesthetics of the nasal tip, we must consider four interdependent elements: volume, geometry, rotation, and projection (Fig. 9-1). For the droopy tip, the principal concerns are rotation—referring to the vertical orientation of the tip—and projection—its forward extension from the face. These elements are often deficient or unfavorable in patients presenting with a drooping nasal tip.
The relationship among these factors is well illustrated in Figure 9-1, where changes in rotation often affect projection and vice versa. An effective surgical plan must respect these dynamic relationships, seeking to optimize rotation while maintaining appropriate projection and tip support.
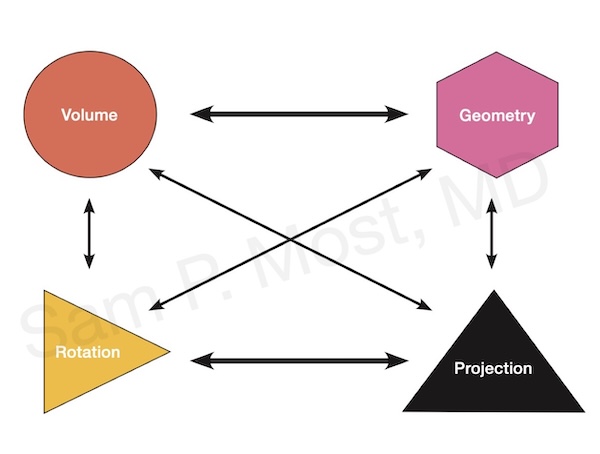
Figure 9-1: Tip rotation and projection relationships.
Structural Basis: The Tripod Concept
The tripod theory (Fig. 9-2) remains a useful conceptual model for tip support. The two lateral crura and the conjoined medial crura function as three legs of a tripod. Adjusting the length or orientation of any of these legs alters tip rotation and projection. For example, shortening the lateral crura increases rotation, while lengthening the medial crura increases projection. This biomechanical model forms the basis for nearly all tip-modifying maneuvers discussed in this section.
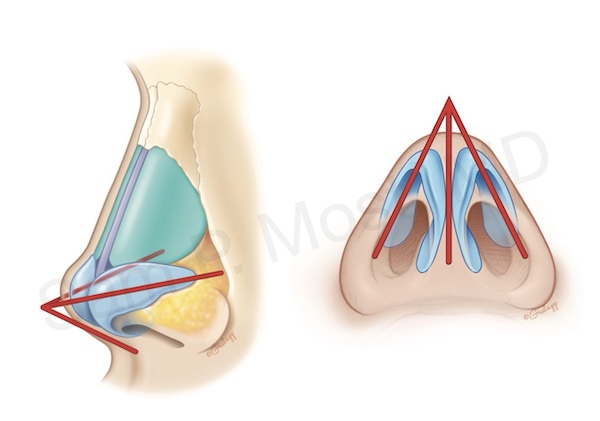
Figure 9-2: Tripod model showing tip support anatomy.
Surgical Approaches to the Droopy Tip
Suture Techniques
Lateral crural steal is a method to effectively reduce the length of the lateral crus (steal) and add to the medial crus (Figure 9-5). This therefore increases tip projection and rotation.
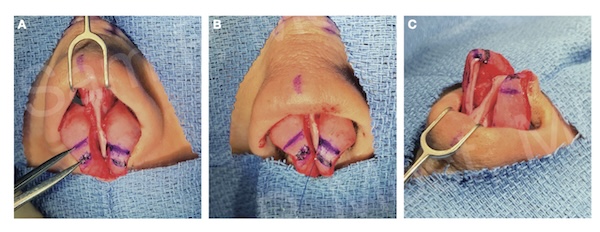
Figure 9-5: Lateral crural steal technique for tip repositioning.
Tongue-in-Groove (TIG) Technique
The TIG technique is a foundational method for tip rotation. In this approach, the medial crura are advanced and secured onto the caudal septum, allowing for precise control of both rotation and projection. Dr. Most has published extensively on this method. When performed correctly, TIG creates a strong central support mechanism that enhances both aesthetic and functional outcomes.
The correct method of TIG is demonstrated schematically in Figure 9-6, where suture placement is diagrammed. Figure 9-8 shows a patient with a droopy tip that was successfully rotated using TIG, with improved nasal base projection and tip angle. Similarly, Figures 9-9 and 9-10 further illustrate the effectiveness of TIG alone or in combination with other maneuvers for correcting downward tip rotation while maintaining structural integrity.
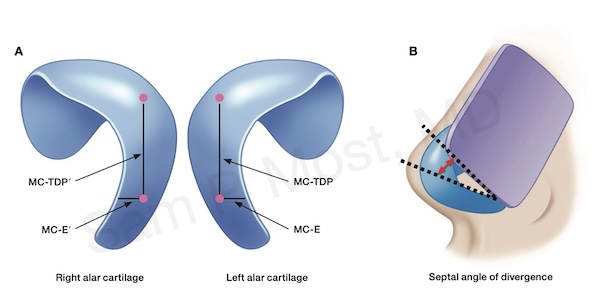
Figure 9-6: Schematic of TIG suture positioning.
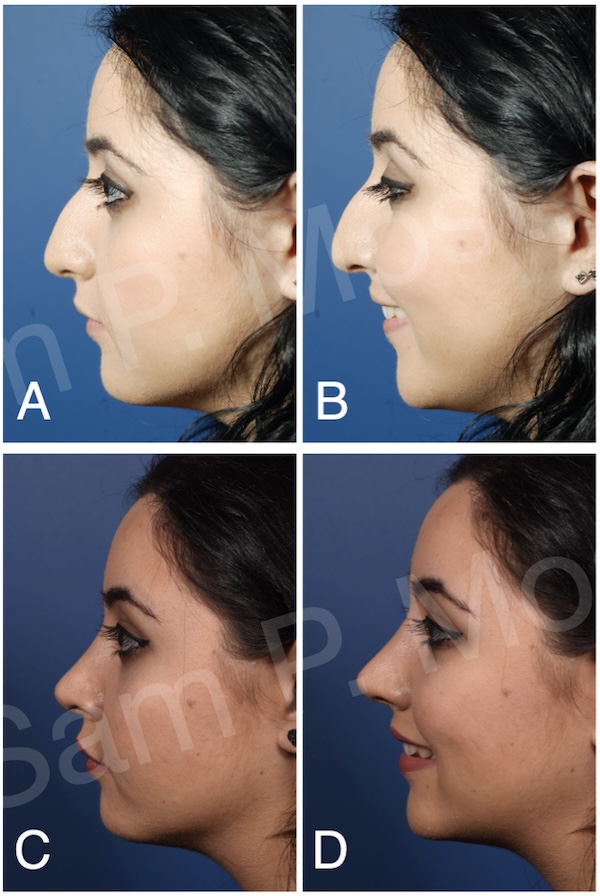
Figure 9-8: Example of patient with improved tip using TIG.

Figure 9-9: TIG used to improve projection and support.
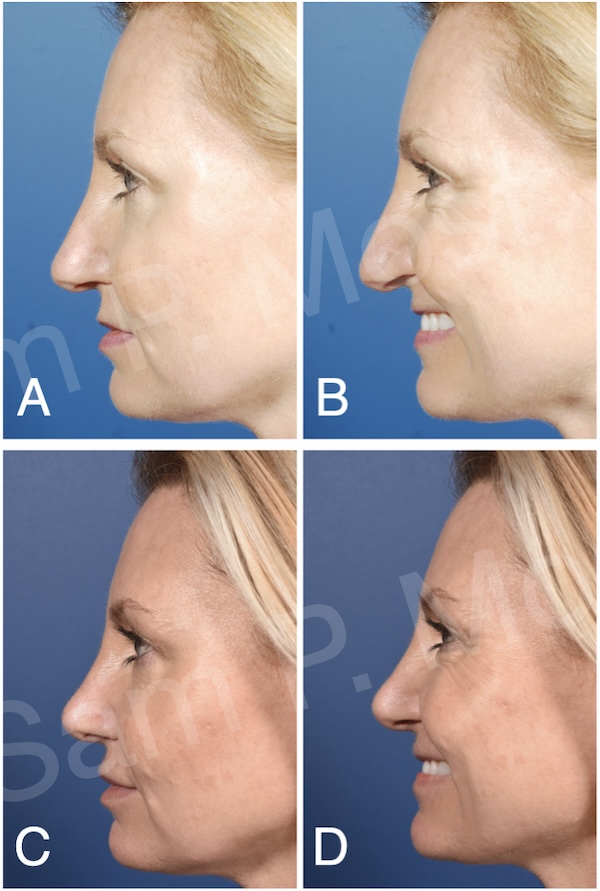
Figure 9-10: Further example of TIG in clinical use.
Septal Extension Grafts (SEGs)
SEGs provide a powerful method for long-term control of both tip projection and rotation. A SEG is a rigid strut that extends from the septum and serves as a platform to which the medial crura can be fixed. This technique is especially useful in revision cases or when the native septal support is insufficient.
As shown in Figure 9-10 (SEG schematic), the SEG can be placed in-line or side-to-side with the septum. In panel A, an in-line septal extension graft maintains both projection and is supported with spreader grafts. In panel B, a side-to-side graft is secured with three permanent sutures.
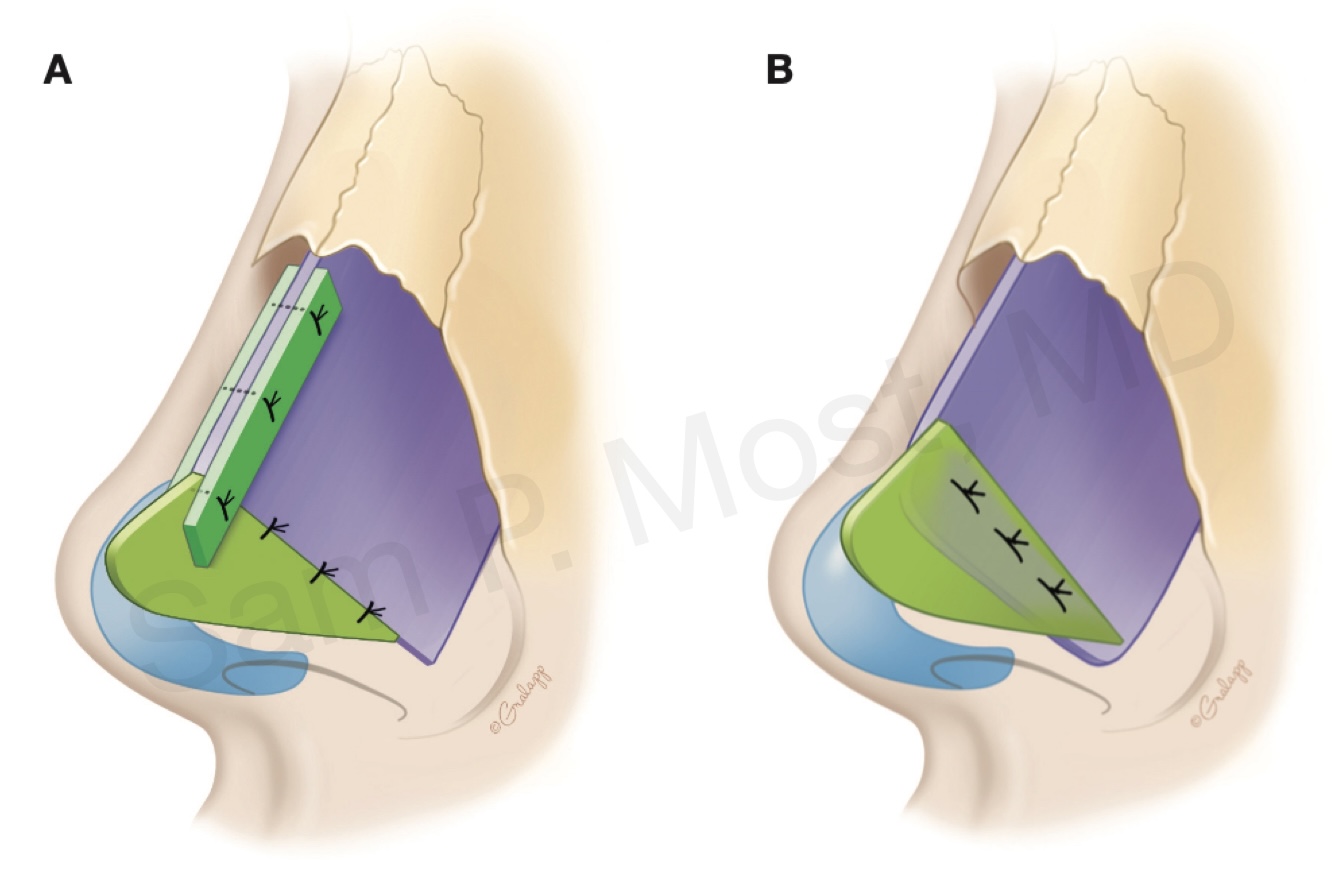
Figure 9-10: Septal extension graft options (in-line vs side-to-side).
Modifying the Lateral Crura
In patients where the lateral crura are overly long, further tip rotation can be accomplished by direct modification of these cartilages.
Lateral Crural Overlay (LCO)
Lateral crural overlay is a technique that effectively shortens the length of the lateral crus, thereby inducing upward rotation and deprojection (remember the tripod!). In this method, a segment of the lateral crus is overlapped and sutured, reducing its length and shifting tip orientation.
Figure 9-13 demonstrates this principle, while Figure 9-14 shows a step-by-step intraoperative view of the LCO technique. Cartilage is cut, overlapped, and secured, with care taken to maintain symmetry and smooth contour. LCO is particularly effective when combined with TIG or SEG in patients requiring significant tip rotation.
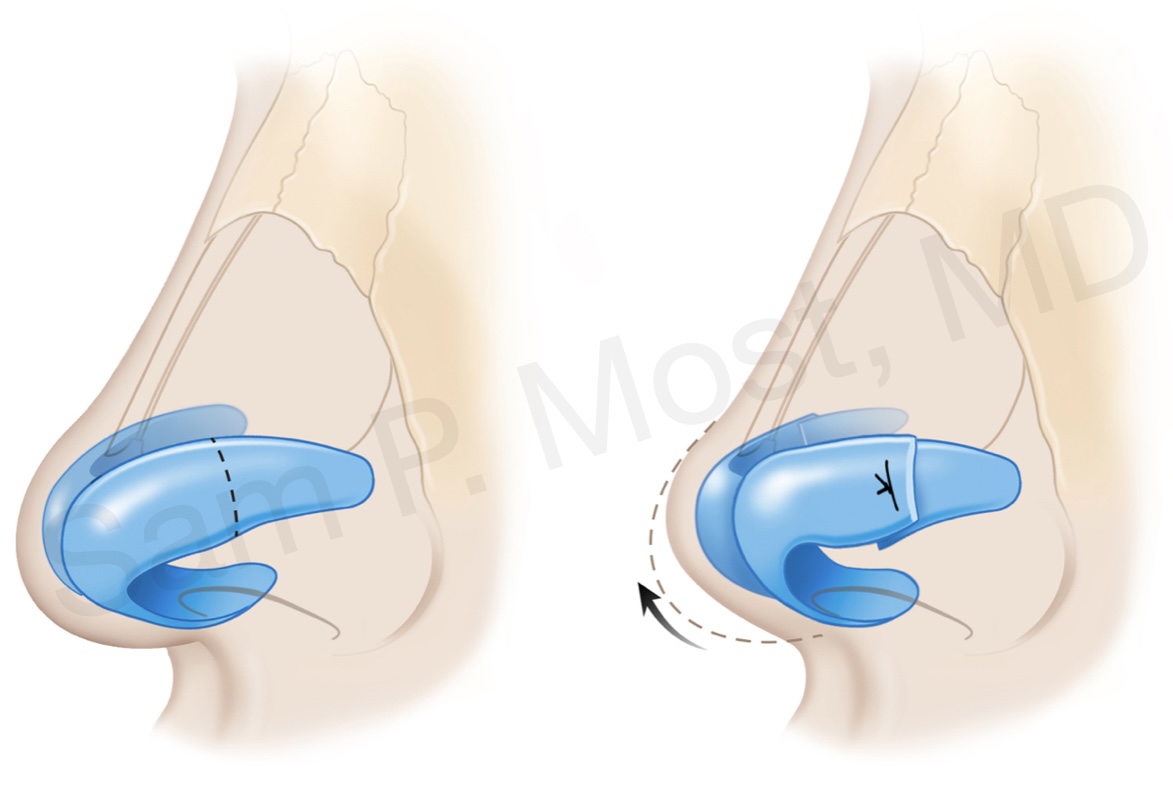
Figure 9-13: Lateral crural overlay schematic showing shortened cartilage.
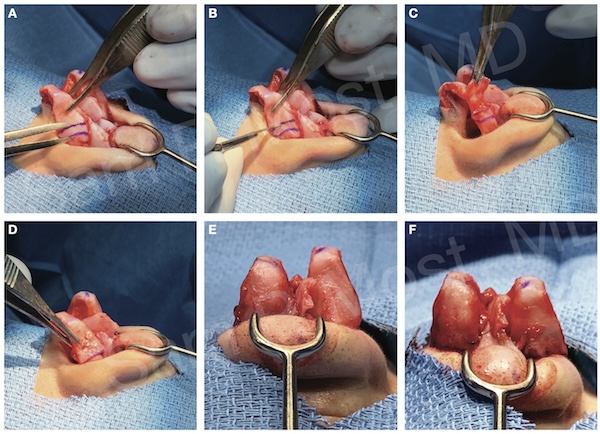
Figure 9-14: Intraoperative view of lateral crural overlay steps.