Revision Rhinoplasty
Structural Approaches to Secondary Nasal Surgery (Educational Overview)
This page summarizes surgical concepts for trainees and colleagues; it is not intended as medical advice.
1. Overview of Revision Rhinoplasty
Revision rhinoplasty represents one of the most challenging areas in nasal surgery, requiring a deep understanding of nasal anatomy, prior surgical effects, and tissue behavior over time. Patients often present with aesthetic dissatisfaction, functional compromise, or both. Common deformities include saddle nose, tip asymmetries, alar retraction, irregularities from over-resection, and dorsal collapse. Scar tissue, poor skin quality, and lack of structural support further complicate the reconstructive landscape.

Preoperative and postoperative appearance following revision rhinoplasty, with diced cartilage dorsal reconstruction.
The goals of revision surgery extend beyond reshaping the nose — it often involves restoring structural support, reestablishing airway function, and improving skin-soft tissue relationships. Each case must be approached as unique, especially in tertiary or quaternary revisions where normal anatomic landmarks may no longer exist.
Effective planning depends on a comprehensive analysis of the deformities, detailed patient history (including operative reports if available), and high-resolution photographs. Equally important is managing patient expectations — surgical correction is often a process of trade-offs, and perfection is rarely achievable. However, functional and aesthetic improvement is very often possible.
In the textbook, Dr. Most shares his extensive experience in revision rhinoplasty. Here is a brief overview with review of a few cases.
2. Grafts in Revision Rhinoplasty
Structural grafting forms the cornerstone of revision surgery. Since native cartilage is often depleted, surgeons must harvest and sculpt autologous materials with precision. The types of grafts used in revision rhinoplasty include septal, conchal (ear), and costal (rib) cartilage — each with its own advantages and limitations.
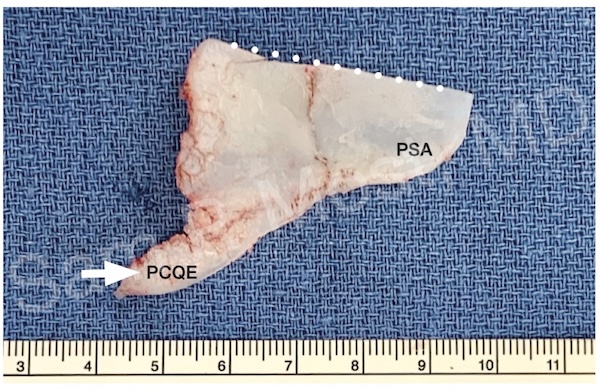
Fig. 16-2. Harvested septum for grafting.
Fig. 16-2 demonstrates a harvested septum. While septal cartilage is ideal due to its straightness and central location, it is often unavailable in revision cases. When present, even small residual segments may be salvaged for minor grafting needs.
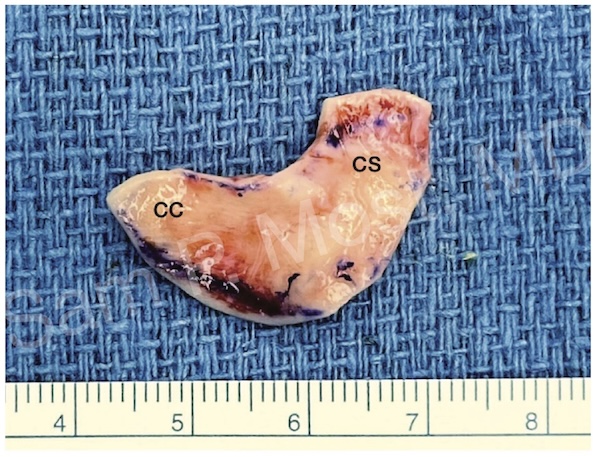
Fig. 16-3. Auricular (ear) cartilage harvest.
Fig. 16-3 shows auricular (ear) cartilage, commonly harvested from the conchal bowl. It has natural curvature, making it useful for alar rim grafts and minor contour refinements. However, its flexibility limits its utility in structural dorsal or septal reconstruction.
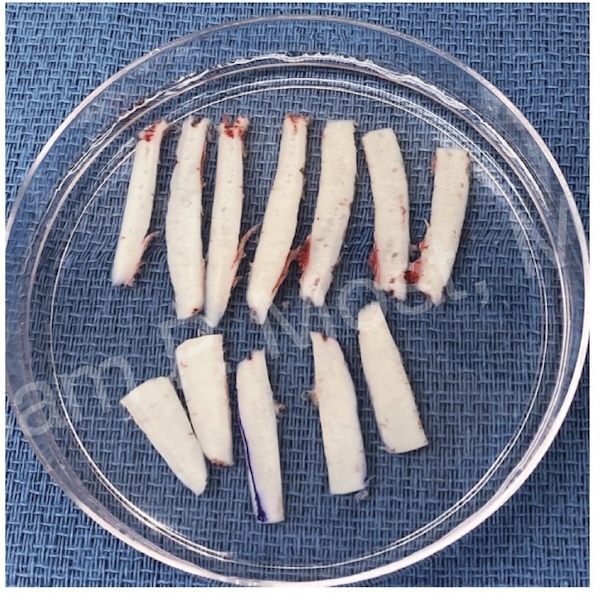
Fig. 16-14. Obliquely cut rib graft for structural use.
Fig. 16-14 depicts costal (rib) cartilage harvested with an oblique cut technique. Rib cartilage offers abundant material and rigidity for robust grafting needs. Warping is a known risk, which can be minimized through precise carving and techniques like balanced cross-sectional (oblique) cuts. Additionally, there is a 1% risk of pneumothorax with rib grafting. The most common issue is pain at the harvest site.
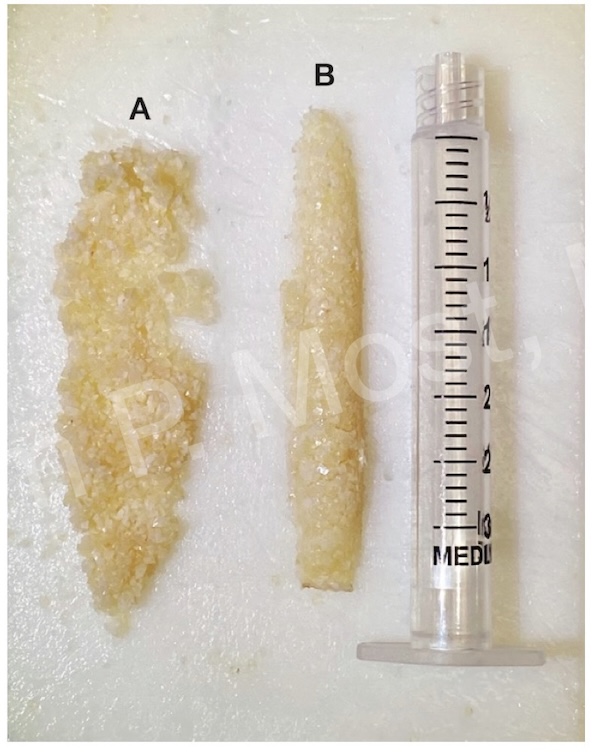
Fig. 16-24. Diced rib cartilage with fibrin glue for dorsal reconstruction.
Fig. 16-24 demonstrates diced cartilage mixed with fibrin glue — a moldable material used for dorsal reconstruction. Unlike traditional "Turkish delight" methods (which use Surgicel), this technique uses fibrin glue to hold diced cartilage together in a sculptable mass. This allows the surgeon to rebuild the dorsum with soft contour and volume control, especially in patients with irregularities or over-resection.
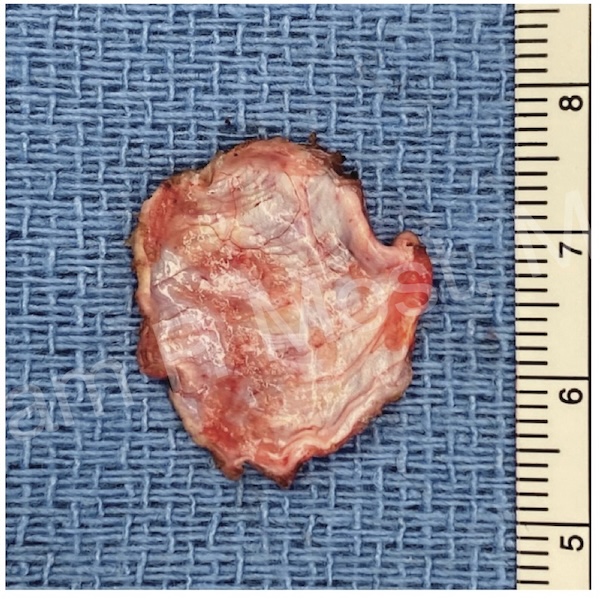
Fig. 16-8. Temporalis fascia for soft-tissue camouflage.
Fig. 16-8 presents the use of temporalis fascia — a thin, pliable material ideal for soft-tissue camouflage. It’s often used over diced cartilage or for smoothing dorsal edges in thin-skinned patients.
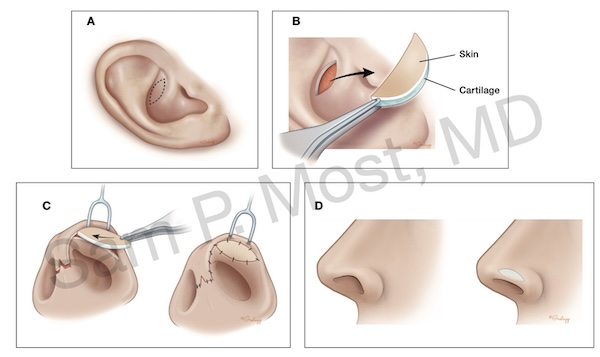
Fig. 16-9. Composite ear graft (cartilage + skin).
Fig. 16-9 shows a composite graft from the ear, which includes both skin and cartilage. These are typically used to correct alar retraction or rim notching when soft tissue and cartilage are both deficient. Composite grafts provide volume, support, and coverage in a single unit.
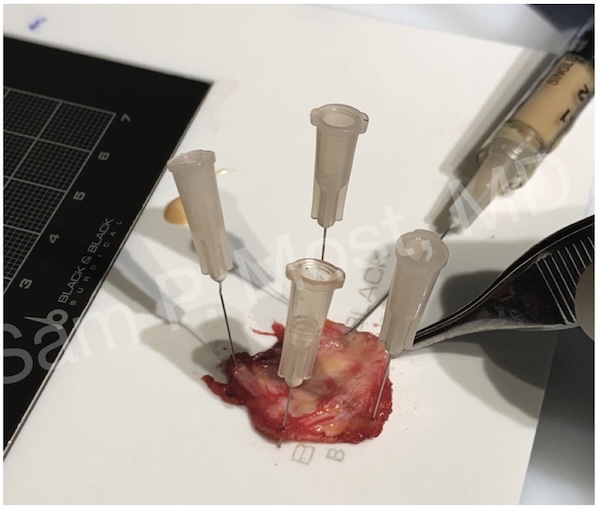
Fig. 13-1. Nanofat injection for skin softening and scar improvement.
Fig. 13-1 depicts nanofat grafting, which involves emulsified fat placed into the soft tissue envelope. While not structural, nanofat improves skin quality, reduces scar density, and enhances contour in compromised or irradiated tissues.
3. Constructing the Framework
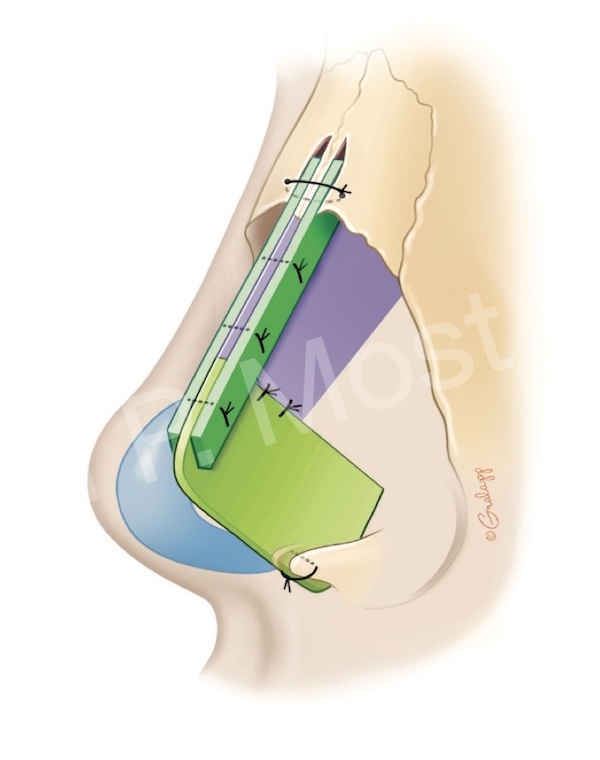
Fig. 12-3. Extended spreader grafts sutured to a septal extension graft.
When traditional septal support is missing, surgeons must reconstruct a central support system from available materials. This often means reconstruction of the tripod of the nose.
Fig. 12-3 shows extended spreader grafts sutured to a septal extension graft. These grafts reestablish the middle vault, widen the internal valve angle, and serve as dorsal scaffolding for camouflage grafts or diced cartilage applications. In revision cases, combining SEG and spreader grafts provides the strength and length required to reshape a previously collapsed nose.
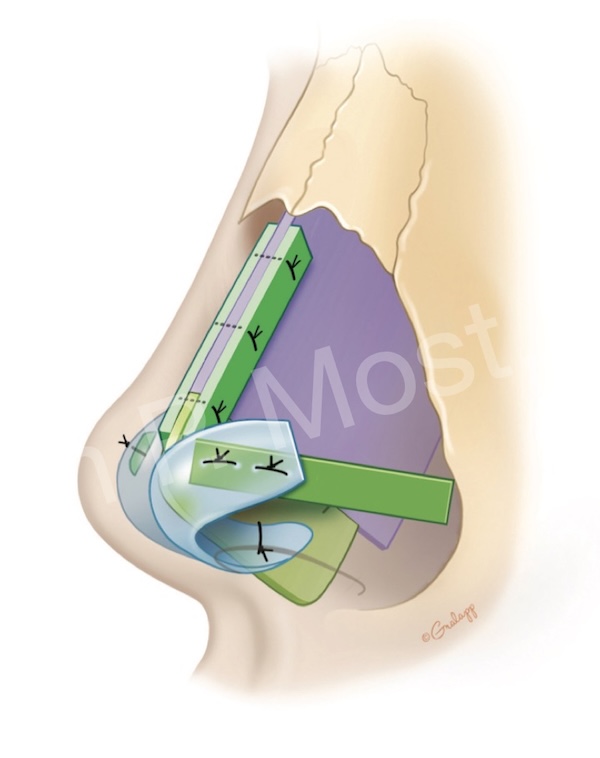
Fig. 11-11. Tetrapod graft reconstruction of caudal, dorsal, and lateral support.
The tetrapod reconstruction method — shown in Fig. 11-11 — is an innovation to recreate all dimensions of the lower 1/3 of the nose. This structural repair recreates the septum with a dorsal strut, caudal extension, and bilateral spreader arms. This construct allows a stable, midline axis for the entire nasal framework. It supports dorsal grafts, resists deviation, and permits fixation to the maxillary spine or anterior nasal spine.
4. Clinical Cases in Revision Rhinoplasty
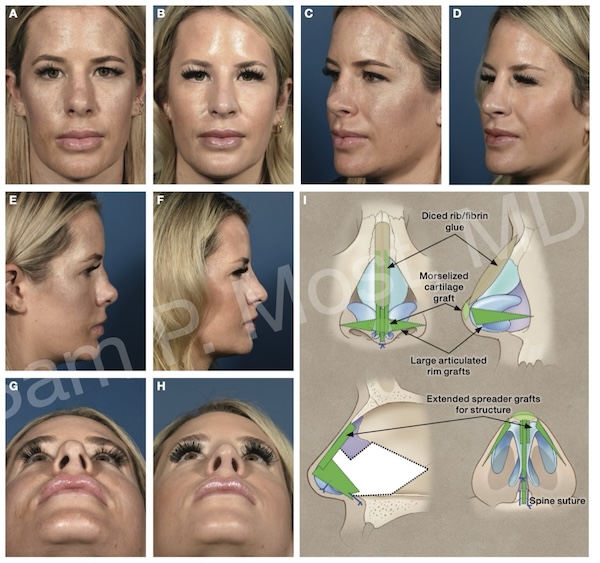
Fig. 12-6 A–I. Tertiary rhinoplasty with autologous rib reconstruction.
Case 1: Shortened Nose with Saddle Deformity
Preoperative and 6-month postoperative images of a tertiary rhinoplasty patient with autologous rib reconstruction. The patient’s first rhinoplasty was complicated by infection, resulting in septal loss (only a 5 mm caudal strut remained with discontinuity in the dorsal strut), nasal shortening, saddle deformity, and medial crural discontinuity. Reconstruction involved tetrapod reconstruction with obliquely cut rib for extended spreader grafts, caudal septal reconstruction, and alar replacement grafts. The anterior septal replacement graft was suture fixated to the maxillary spine. Dorsal reconstruction involved bony rasping (followed by osteotomies to close an open roof) and replacement of the entire dorsum with diced rib/fibrin glue. A tip graft made of morselized cartilage was placed.
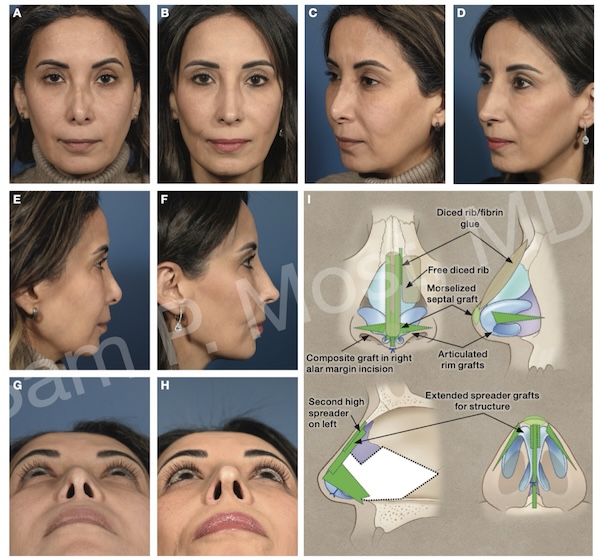
Fig. 12-7 A–I. Multiply operated nose with diced rib and tetrapod reconstruction.
Case 2: Over-Resected and Multiply Operated Nose
Preoperative and 12-month postoperative images of a patient who had tertiary rhinoplasty with tetrapod reconstruction. The caudal septum was resected and an ASR graft was placed. Dorsal strut support and contour was provided with extended spreader grafts and onlay diced rib/fibrin glue. A second, higher spreader was placed on the left to support a medially displaced nasal bone. Free diced cartilage was also placed on the left nasal sidewall where the nasal bone had collapsed. Bilateral articulated rim grafts were secured to the tip construct, and the tip was camouflaged with a thin septal (morselized) cartilage graft. A small composite graft (6 × 3 mm) was harvested from the right concha symba and placed along the medial right nostril edge for slight asymmetric retraction.
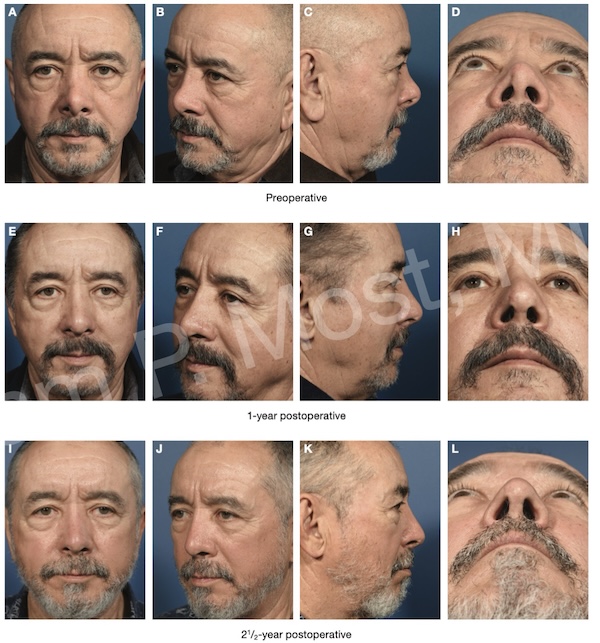
Fig. 12-8 A–L. Over-shortened nose post-primary rhinoplasty with long-term follow-up.
Case 3: Over-Shortened Nose with Overresection of the Bridge and Nasal Obstruction
Preoperative and 1-year and 2½-year postoperative photos of a patient who presented for secondary rhinoplasty after dorsal overresection and overly shortened nose.
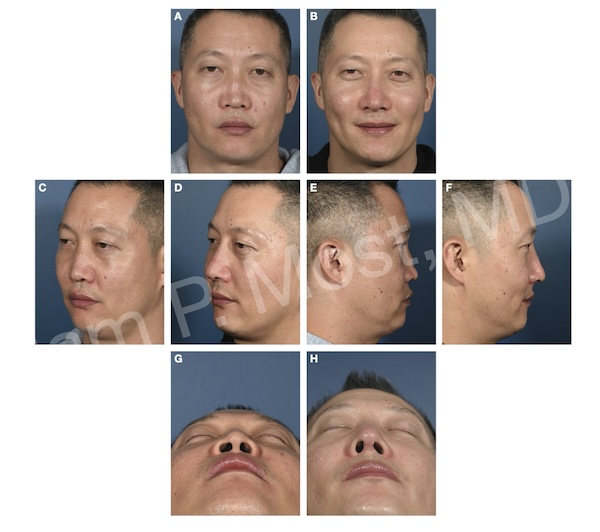
Fig. 12-10 A–H. Saddle nose deformity reconstruction following septal perforation.
Case 4: Saddle Nose Deformity
Preoperative and 6-month postoperative images of saddle-nose reconstruction. The patient suffered a septal perforation and saddle deformity before presenting for reconstruction. The septal perforation was clean and too large for repair; thus, it was not reconstructed.