Wide Tip
Understanding Tip Aesthetics: Volume and Geometry
This page summarizes surgical concepts for trainees and colleagues; it is not intended as medical advice.
Tip aesthetics are governed by an interplay of four core concepts: volume, geometry, rotation, and projection. These elements are not independent; changes in one will inevitably affect the others (Fig. 10-1). However, for the purposes of managing the wide tip, we focus primarily on volume—the physical bulk of the tip—and geometry—its shape and contour. The visual impression of a wide nasal tip may stem from excess volume, unfavorable cartilage configuration, soft-tissue redundancy, or all three.
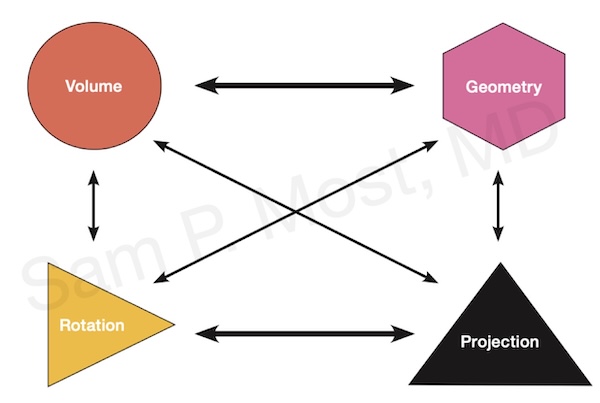
Figure 10-1: Core concepts in tip dynamics — projection, rotation, volume, geometry.
A crucial first step in assessing the wide tip is determining whether the tip is cartilage-predominant or soft-tissue skin envelope (SSTE)-predominant. As depicted in Figure 10-2, this distinction helps guide which techniques are likely to be most effective. Patients with thicker skin or a bulkier SSTE may require debulking or camouflage strategies, while maintaining or projecting the tip, while those with thin skin and strong cartilage support may benefit more from cartilage modification or suture techniques, keeping an eye on reducing the risk of irregularities that may become visible over time.
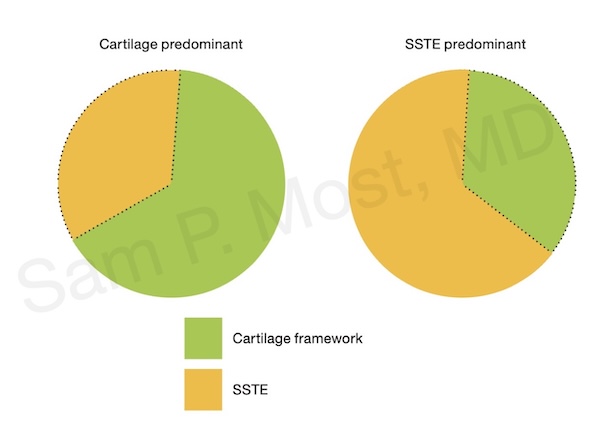
Figure 10-2: Tip classification based on soft-tissue vs cartilage dominance.
Wide variation in tip cartilage contours
The tip cartilages are quite heterogenous in morphology as illustrated in Figure 10-7: Top left: Asymmetric cartilages with excess vertical height (right is concave, left is convex). Top right: Lateral crura convexity (bulbous or boxy appearance). Bottom left: Lateral crura malposition (cephalically oriented—see later below). Bottom right: Wide, convex lateral crura with thin, weak medial crura. Understanding which of these contributes to the deformity is essential to crafting an effective surgical plan.
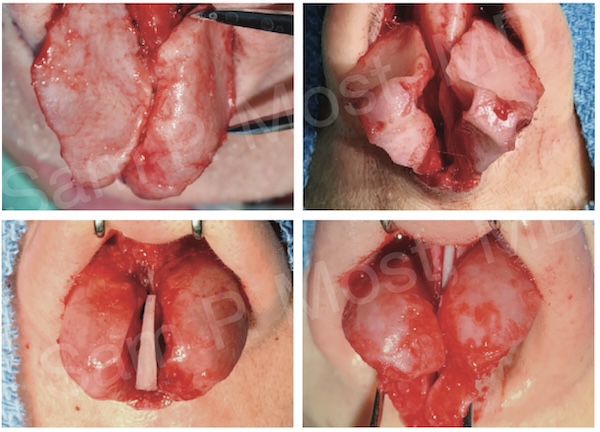
Figure 10-7: Common variants in tip cartilage morphology.
Techniques for Cartilage-Predominant Wide Tips
Cephalic Trim and Cephalic Turn-In
A classic and reliable technique for reshaping wide lateral crura is the cephalic trim. By removing the upper segment of the lateral crus, the tip volume can be decreased (Fig. 10-8). In older textbooks, it was recommended that 3–4 mm be preserved, and that cutting the ‘rim strip’ was acceptable. Today, we recommend conserving 7 or more mm, depending on cartilage strength, and do not cut the strip (excepting in cases of overlap or grafting).
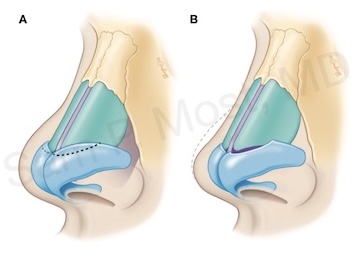
Figure 10-8: Cephalic trim removes upper lateral crura for narrowing.
As shown in Figure 10-10, the cephalic turn-in principle is taken further with a cephalic turn-in flap, wherein the trimmed segment is folded under and sutured to the remaining cartilage, reinforcing the margin and improving strength and definition.
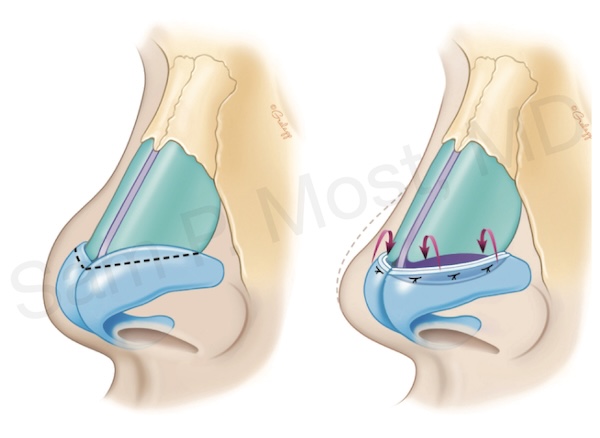
Figure 10-10: Cephalic turn-in technique folds cartilage for support and narrowing.
This approach provides tip narrowing while preserving—and often enhancing—structural support. Its effectiveness is shown in Figure 10-14, where a patient’s tip is narrowed using cephalic turn-in alone, without grafting.
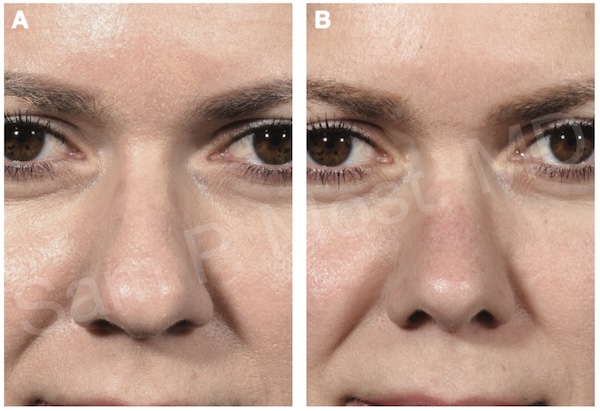
Figure 10-14: Clinical result from cephalic turn-in without grafts.
Suture Techniques: Transdomal and Interdomal
Modified transdomal sutures are employed to change tip geometry by narrowing the domal angle and softening the tip contour (Fig. 10-40). These sutures can be combined with interdomal sutures to bring the domes closer together, particularly in cases of excessive interdomal distance. When placed precisely, they offer finesse in shaping the supratip and defining the angle of divergence between the domes.
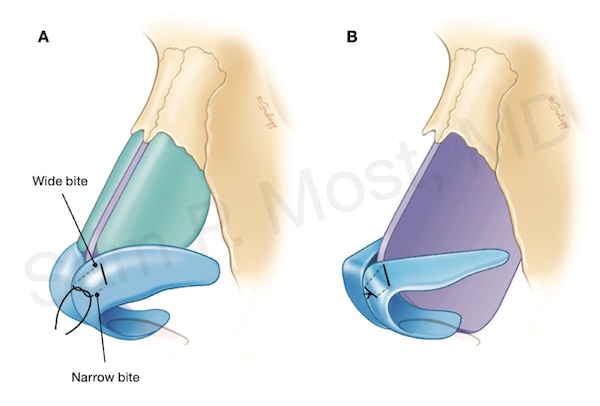
Figure 10-40: Transdomal sutures narrow domal angle and soften contour.
In Figure 10-53, a patient’s wide tip is successfully narrowed with transdomal and interdomal suturing alone, demonstrating the power of these soft techniques in well-selected cases.

Figure 10-53: Tip narrowed with transdomal and interdomal sutures.
Alar Spanning Sutures
Alar spanning sutures, illustrated in Figure 10-47, are another subtle yet powerful suture tool for altering the curvature of the lateral crus and supporting a narrowed tip. They can be especially useful in adjusting supratip contour and fine-tuning rotation.
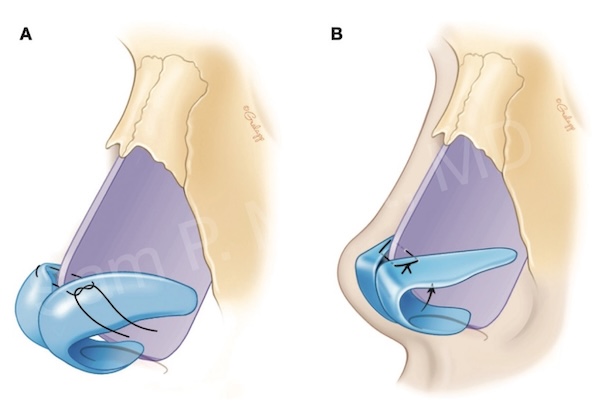
Figure 10-47: Alar spanning suture to reshape lateral crura.
Lateral Crural Repositioning
When the lateral crura are convex or malpositioned, repositioning techniques can be beneficial. The lateral crural repositioning method involves detaching and reorienting the lateral crura medially. This allows the cartilages to sit in a flatter, more favorable plane.
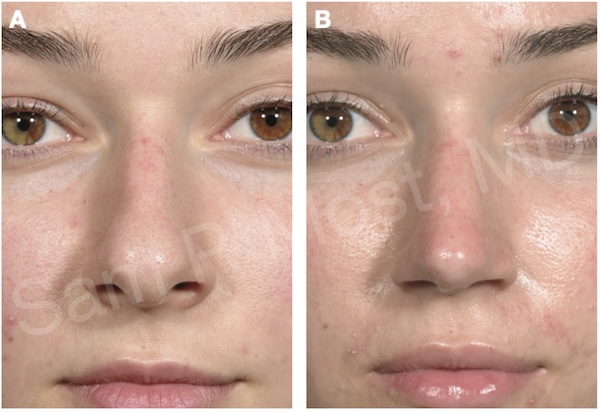
Figure 10-24: Lateral crural repositioning to improve contour and narrow the tip.
Lateral Crural Strut Grafts (LCSG)
The LCSG provides structural flattening and reinforcement of the lateral crus, particularly when intrinsic convexity resists manipulation. A standard LCSG is illustrated in Figure 10-16, where a flat graft is placed deep to the lateral crura, correcting concavity or convexity and allowing for straightening.
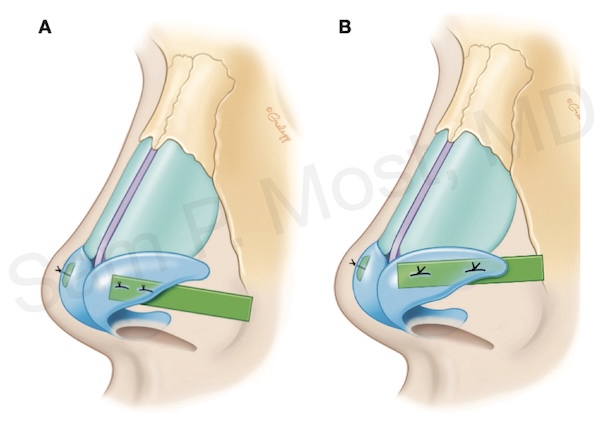
Figure 10-16: Lateral crural strut graft diagram for straightening convex cartilage.
Figure 10-17 shows how a shorter graft, described by Most, the mini-LCSG, can be used when full-length support is unnecessary.
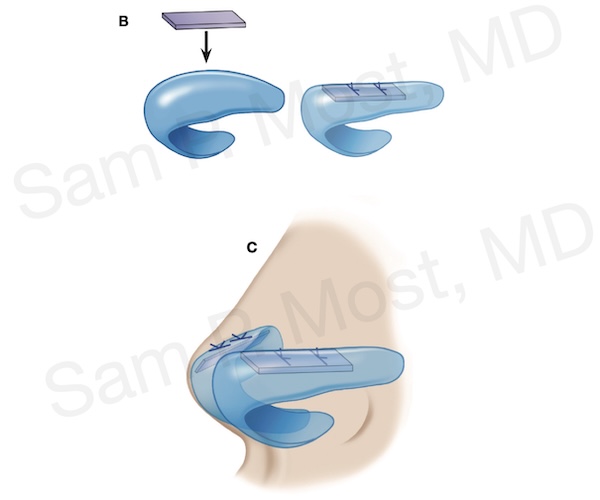
Figure 10-17: Mini–LCSG technique for localized support and straightening.
In Figure 10-20, the mini–LCSG is shown intraoperatively, inserted to reinforce and realign lateral crus curvature.
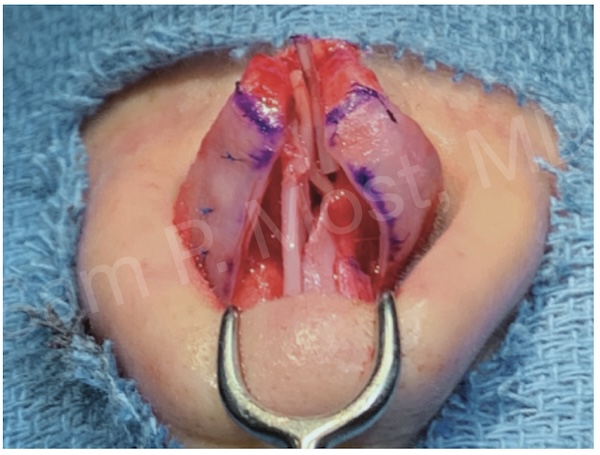
Figure 10-20: Mini–LCSG placed intraoperatively under lateral crura.
A good clinical outcome using this approach is seen in Figure 10-22.
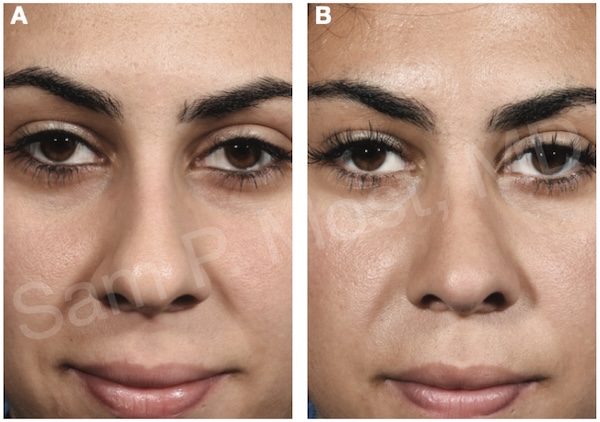
Figure 10-22: Narrowed tip after use of a mini–lateral crural strut graft.
Rim Grafts
Rim grafts serve to buttress and contour the lateral alar margin, reducing shadowing and creating a narrower silhouette (Fig. 10-27). In situations of poor alar support or concavity, these can improve both function and form.
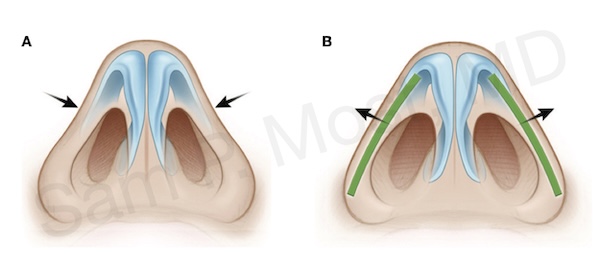
Figure 10-27: Rim graft technique for supporting the alar margin.
Articulated rim grafts differ in that they are sutured (articulated) to the nasal tip. The classic ARG is sutured over the top, while the underlay ARG (uARG) is secured beneath the domal cartilage, as diagrammed in Figure 10-30.
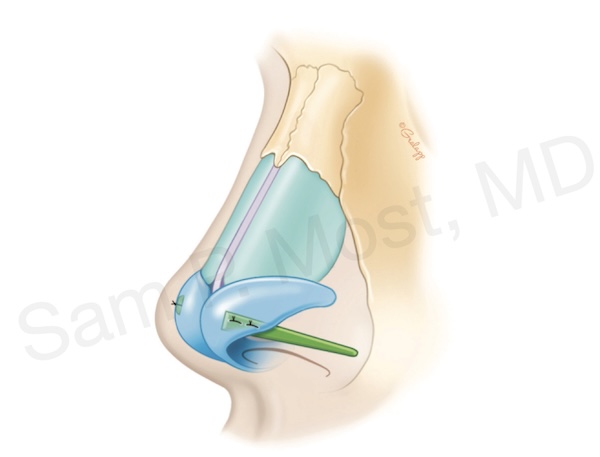
Figure 10-30: Underlay articulated rim graft (uARG) placement diagram.
Figure 10-31 demonstrated a real patient example in which the uARG created a highlight from the tip to alar lobules.
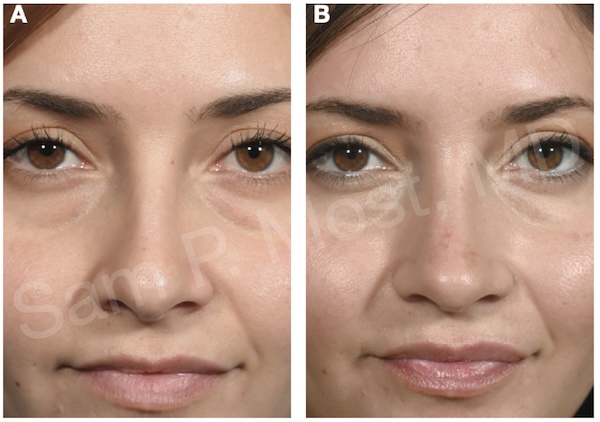
Figure 10-31: Patient result following placement of a uARG.
Techniques for SSTE-Predominant Wide Tips
Soft-Tissue Debulking
In patients with excessive subcutaneous fibrofatty tissue or sebaceous thickening, direct debulking of the tip soft tissue can be performed cautiously. This is often done in conjunction with cartilage-modifying maneuvers to optimize the tip contour.
In Figures 10-56 and 10-57, the patient underwent tip debulking and soft-tissue contouring to achieve narrowing. The reduction of soft-tissue volume unveiled the underlying cartilage work and improved overall tip refinement. Though not shown, the nasal tips were projected slightly to highlight the framework.
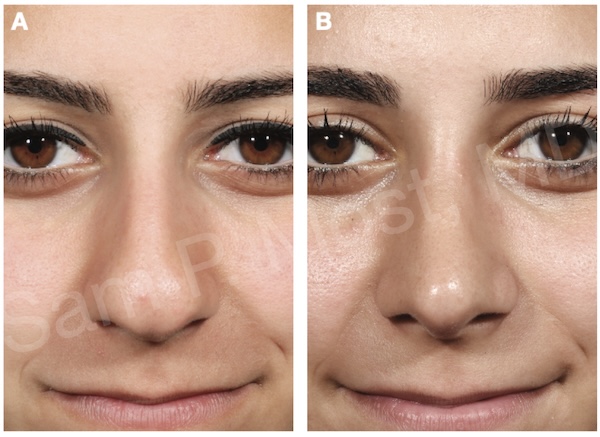
Figure 10-56: Preoperative wide tip with thick SSTE.
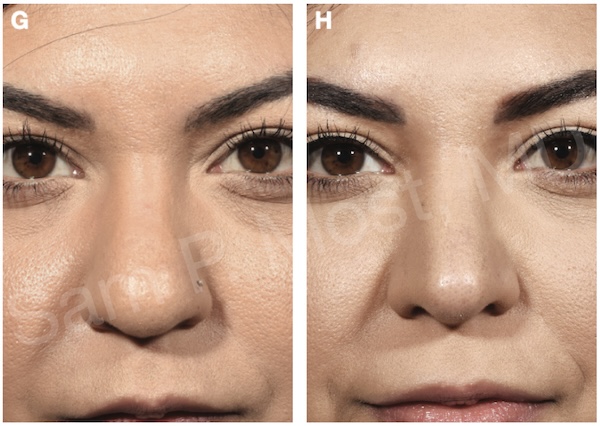
Figure 10-57: Postoperative result after debulking and projection.